We make physician lives better, exceeding their expectations for cash recoveries, coding accuracy, and denial reversals.
The importance of RCM in the evolving healthcare landscape cannot be overstated. It encompasses the entire lifecycle of a patient account, from the initial point of contact and appointment scheduling to the final payment of the balance.In the dynamic and complex terrain of healthcare, effective RCM ensures the financial health and sustainability of healthcare organizations, including innovating primary care organizations and independent primary care practices.
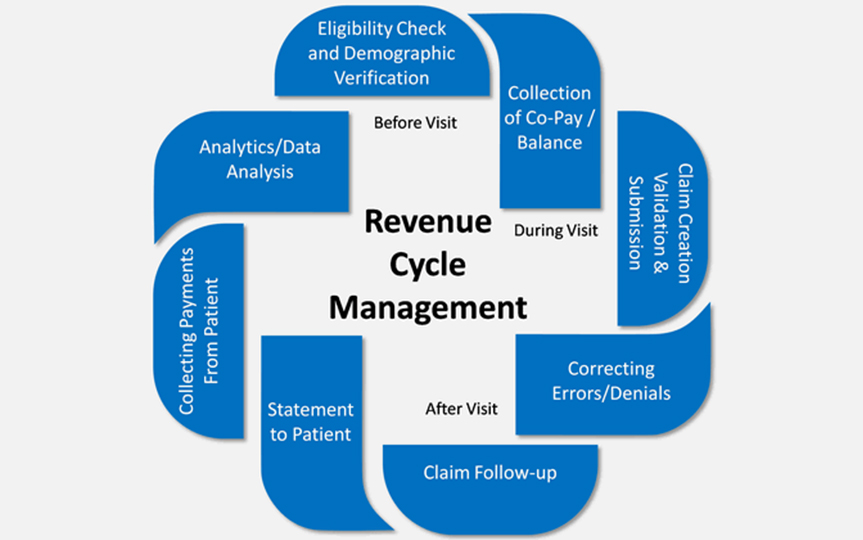
Understanding and optimizing each stage of the Revenue Cycle Management process is essential for healthcare organizations to maximize revenue, minimal financial risks, and provide quality care.
The 13 steps of Revenue Cycle Management process includes:
➢Patient pre-registration: Capture patient demographic, insurance, and eligibility information in real-time.
➢Insurance verification: Verify the patient’s insurance.
➢Patient registration: Register the patient.
➢Charge capture: Capture charges for services rendered.
➢Claim submission: Submit claims to payers like Medicare, Medicaid, and United etc.
➢Claim adjudication: Process claim adjudication.
➢Payment posting: Post payments.
➢Denial management: Review rejections, fix mistakes, and resubmit claims.
➢Accounts receivable follow-up: Manage outstanding patient balances.
➢Patient statement processing: Process patient statements.
➢Patient payment collection: Collect patient payments.
➢Revenue analysis and reporting: Analyze and report revenue.
➢Compliance and auditing: Ensure compliance and conduct audits.
Benefits of Healthcare Revenue Cycle Management with ParaMed
The benefits of effective Healthcare Revenue Cycle Management are far-reaching, impacting both the financial stability of healthcare organizations and the overall quality of patient care.Optimize your healthcare organization’s financial performance and ensure practice sustainability with ParaMed Billing Solutions revenue cycle management features.
➢Enhanced Payer Negotiations: Effective RCM empowers healthcare organizations in payer negotiations. By having a thorough understanding of their financial data and performance metrics, healthcare providers can negotiate more favorable contracts with payers. This includes negotiating better reimbursement rates and terms that align with the organization’s financial goals.
➢Timely and Accurate Reimbursement: A well-orchestrated RCM process ensures that claims are submitted accurately and in a timely manner. This, in turn, accelerates the reimbursement process. Timely submission reduces the likelihood of claim denials and ensures that healthcare providers receive payments promptly, contributing to consistent cash flow.
➢Reduction in Bad Debt: Effective RCM practices help identify and address potential issues with patient payments early in the process. This includes verifying insurance coverage, providing clear communication about patient financial responsibilities, and implementing efficient billing processes. As a result, the risk of bad debt—unpaid or unrecoverable patient balances—is significantly reduced.
➢Increase in Claims Paid After First Submission: A robust RCM process aims for a high rate of claims paid after the first submission. This reduces the need for time-consuming and resource-intensive appeals. When claims are submitted accurately the first time, healthcare organizations can streamline their operations, minimize delays in reimbursement, and enhance overall efficiency.
For more insights and tips on Revenue Cycle Management by ParaMed Billing Solutions, please reach out via email at info@paramedbilling.com or by calling 479-552-5346.